Placenta Accreta Spectrum (PAS): Step-by-Step Surgical Management Guidance
Author
Clinical History
Miss E.F a 35 YO pregnant lady G4P3 previous 3 C/S, GA 35+5. Fit with no medical problems. Pre pregnancy weight= 50 kgs, BMI=19.4. Allergic to penicillin. She presented with multiple episodes of antepartum hemorrhages starting at 26 weeks gestation which led to multiple admissions.
Investigations
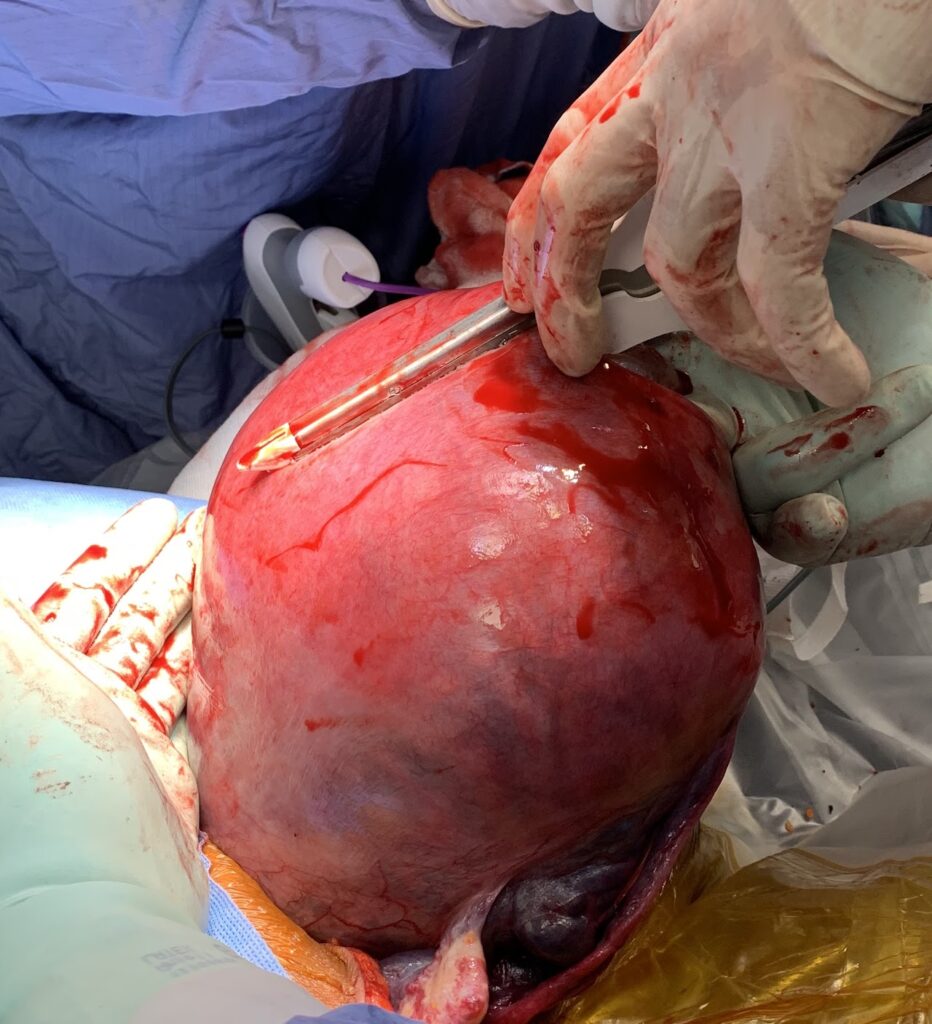
Antenatal ultrasound scan showed an abnormally invasive placentation with evidence of percreta into bladder and parametrium in addition to excessive neovascularity extending down into the cervix and parametrium.
Initial management
Pre surgery multidisciplinary (MDT)plan
- Lower uterine segment C/S
- In view of low BMI, and short stature patient expected to have very low circulating volume, therefore the plan was to minimise blood loss as much as possible.
Surgical plan and assessment
- Newborn: special care baby unit > (SCBU) was booked.
- Team and roles:
- Present: senior anaesthetists, gynaecology surgeon (PAS surgeon to perform surgery), high risk obstetricians (for delivery & USS), midwives, paediatricians, cell salvage team, experienced theatre nursing staff.
- Standby if needed: vascular surgeon, GI surgeon, urology.
- Theatre helicopter:
- senior consultant in obstetrics.
- Responsibility:Observe overall situation and responsible for taking appropriate actions when needed.
- Prepare 4 units of blood.
- Consent her to the risks and complications of the surgery including the risk of death.
- Upper segment (classical) C/S + hysterectom
The surgery
The surgery was divided into two parts
- Deliver the baby
- Hysterectomy (pre decided and patient consented to) , depending on the severity of the PAS with the aim to minimise blood loss during the surgery.
Surgical steps:
Phase 1: Entry, Delivery & Assessment
- Speculum examination without any digital examination. Aim – assess the risk of cervical/vaginal varicosities.
- Midline laparotomy incision and entry to the abdomen.
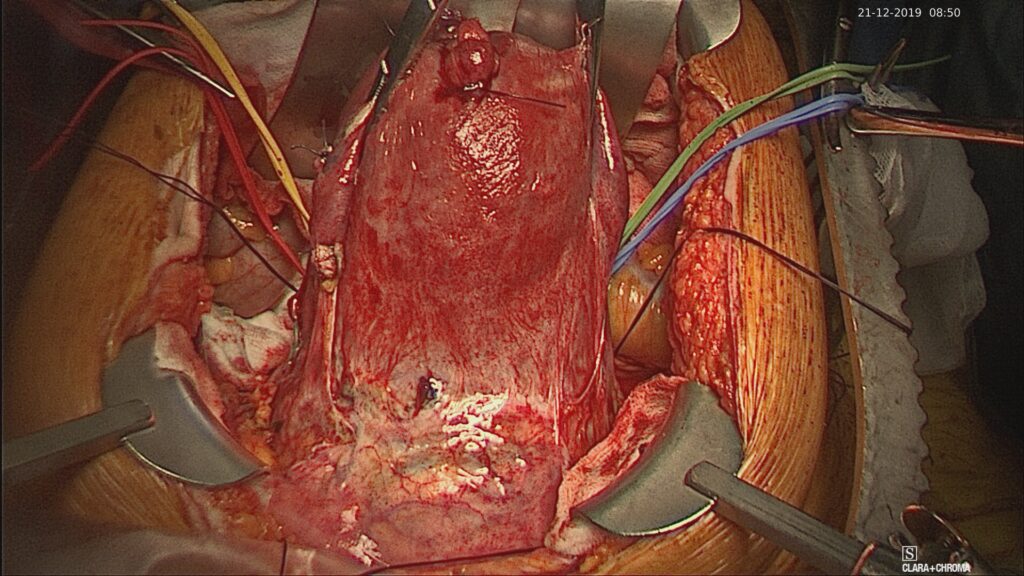
- Examination of the lower segment to assess the severity of PAS – excessive neovascularity, visible evidence of any parametrial invasion, bladder invasion
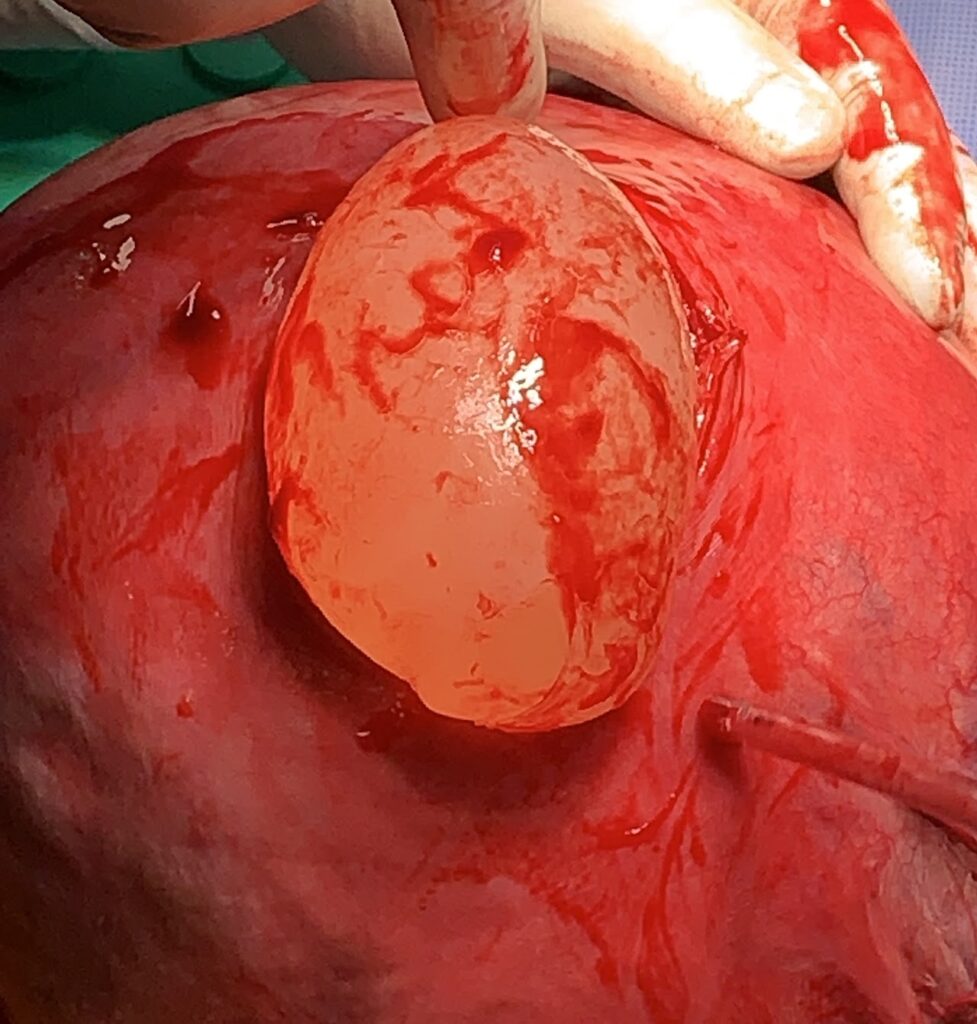
- Intra-operative ultrasound scan. Aim – identify placental location and mark the edge with diathermy.
- Important: No exteriorising of the uterus to minimise the risk of bleeding.
- Uterine incision and delivery:
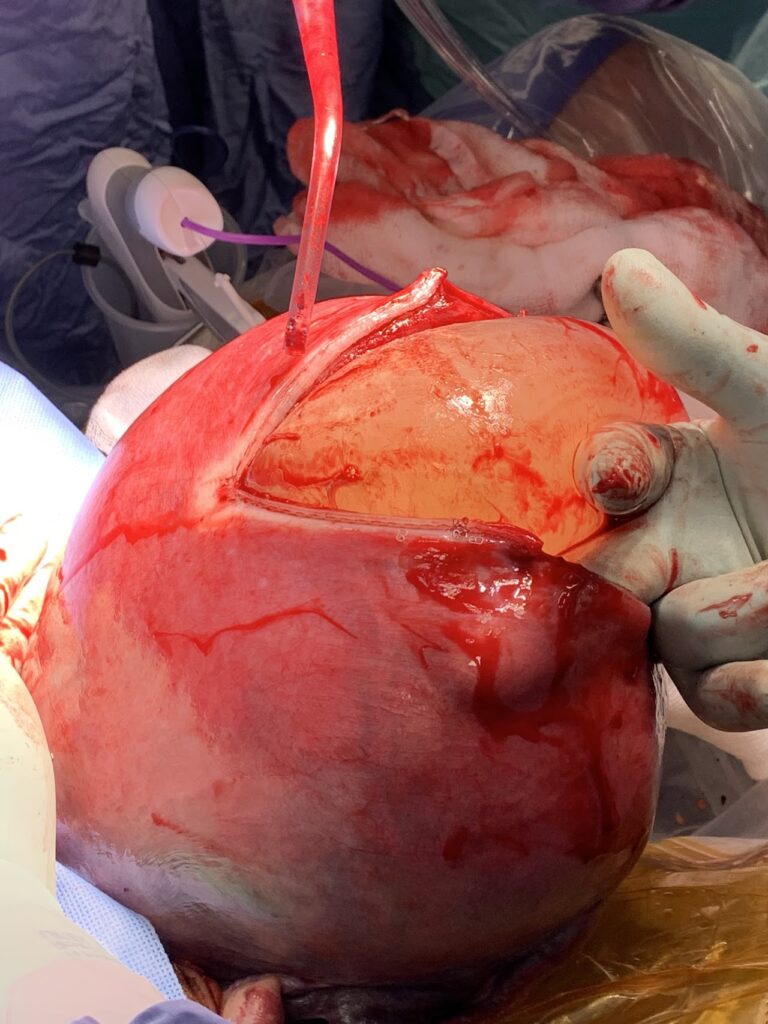
- Fundal incision above the marked placental edge and delaying the cord clamping.
- GIA stapler can be used after small window incision to minimise blood loss from CS edges
- After delivery and cord clamp:
- Avoid uterotonics.
- Allow time for possible spontaneous placental separation so the plan was to go for hysterectomy as AIP was definitely diagnosed.
- Perform dimple sign test
Phase 2: Hysterectomy step-by-step
- Retroperitoneal access and opening pelvic sidewalls to identify key structures.
- Sling the ureters (always), common iliac (if required – depending on severity)
- Apply loose tie to anterior division of the internal iliac arteries (aim – you can tighten immediately in case of excessive bleeding).
- Perform salpingectomy and preserve ovaries
- Bladder reflection.
- Identify the uterovesical fold. Dissection carried on with bipolar scissors.
- Managing abnormal vascularity. Authors preference is to used advanced heamostatic device – Maryland ligature.
- In cases where UV fold is difficult to identify best to fill the bladder 200-300 ml saline (with/without blue dye) while dissecting bladder.
- Tip: use lateral to medial technique with filled bladder to aid difficult bladder dissection
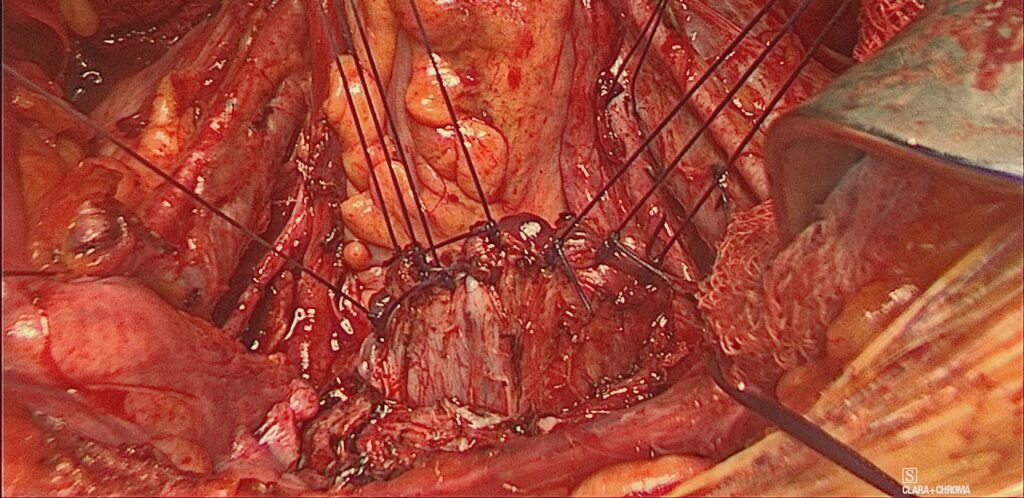
- Colpotomy & vault closure
- Authors preference is to use Zeppelin clamps first then perform the colpotomy using sharp scissors
- We close with monofilament (Monocryl #1) interrupted sutures.
- Abdominal closure and drains
- Authors do not use drains routinely
- Rectus sheath closure: Loop PDS
- Skin closure usually with subcutaneous monocle #3/0
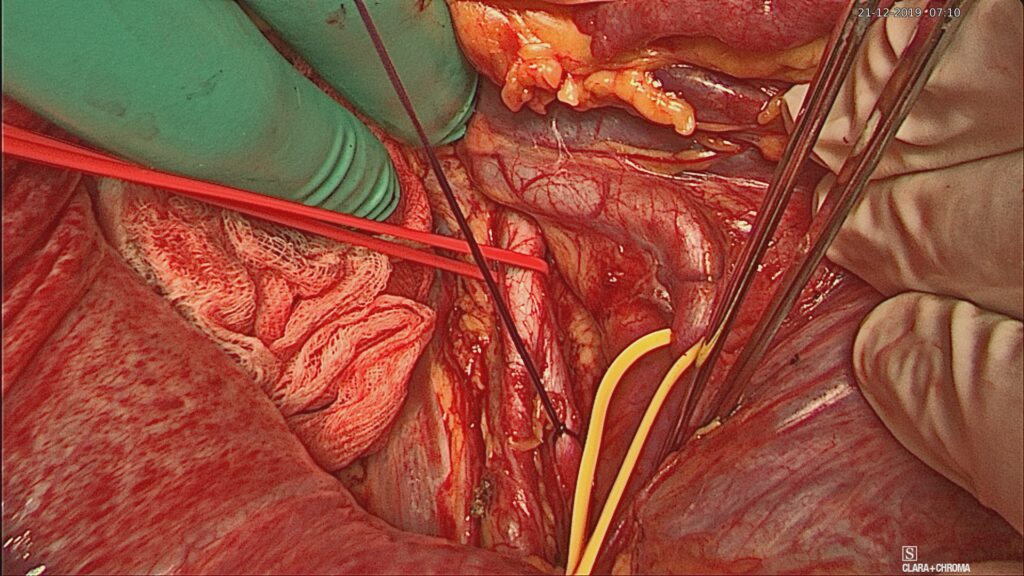
Retroperitoneal access & slinging ureter
Loose tie to anterior division od IIA
Bladder reflection
Colpotomy
Placenta Accreta Spectrum (PAS) Discussion
Definition
Abnormal attachment of the placenta to the myometrium, as a result of the absence of the Nitabuch’s layer which is caused by a defect during the decidual formation.
- Accreta; Complete adherence of the placental villi superficially to the myometrium
- Increta; Deep invasion of the placental villi into the myometrium.
- Percreta; Penetration of the full thickness of the myometrium.
Etiology
The absence of the Nitabuch’s layer which is the fibrinoid deposition between the compact and spongy layer of the decidua basalis.
Risk factors
- History of the previous accreta.
- History of placenta previa.
- History of abortions.
- Surgical trauma to the uterine endometrium or the superficial myometrium such as
D&C, manual removal of placenta, postpartum endometritis or myomectomy. - Previous C/S and other uterine surgeries.
- Advanced maternal age (>35) and assisted reproductive technology.
- Uterine structural defects such as the bicornuate uterus, adenomyosis, submucous fibroids, and myotonic dystrophy.
Epidemiology
- A previous C/S increases the risk of invasive placentation up to seven-folds.
- One half to two-thirds of patients will remain undiagnosed during the pregnancy
Diagnosis and Management
Diagnosis
- Antenatal diagnosis of patients with high suspicion of developing placenta accreta.
- Ultrasound is highly accurate but operator dependent.
- MRI can be used to assess the depth of invasion and the lateral extension of myometrial invasion.
- Women with previous C/S and anterior low-lying placenta must be screened for placenta accreta.
Management
- MDT with expertise in diagnosing and managing invasive placentation.
- Delivery at the 35 to 36+6 weeks of gestation.
- Plan an emergency delivery
- Gather a team of senior anaesthetists, obstetricians, and gynaecologists experienced in managing AIP.
- Prepare blood, 8 units or more.
Treatment options
- Hysterectomy.
- Leaving placenta in situ ( conservative – no surgical intervention)
- Focal segment resection (uterine preservation)
Complications
- Massive obstetric hemorrhage.
- Lower urinary tract damage.
- The need for blood transfusion.
- Uterine rupture in the case of Percreta.
